Making 3D printed implants for children with ear deformities
Over 100,000 children enter the Royal Hospital for Sick Children (known also as “The Sick Kids”) annually. Located in Edinburgh, its facilities attend to children like Ellie, who suffers from a congenital malformation of the ear’s elastic cartilage. Doctors call this “microtia,” a medical term that translates from Latin as “abnormal smallness of the ear.” For some with this condition, the pinna (or external ear) can be so small as to appear practically non-existent. And due to the underdevelopment of both the middle ear and external canal, microtia is often accompanied by some level of hearing impairment. With 1 out of 6,000 babies born with this condition, at least 10 young patients from Scotland stand to have a problem similar to Ellie’s. And that’s only in Scotland in a single year.

Entrance to the Royal Hospital for Sick Children.
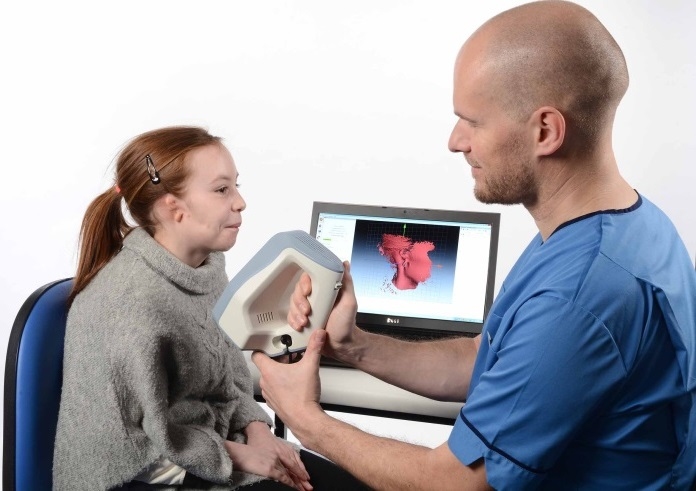
Clinical nurse specialist, Kerr Clapperton using Artec Spider to scan Ellie's ear in Artec Studio.
Fortunately, Edinburgh is home to Ken Stewart, who in addition to his long list of other professional appointments, heads the local Ear Reconstruction Service of Scotland. There he has been fine-tuning ways to perform reconstructive surgery on both children and adults afflicted with ear malformations.

NHS lead clinician and head of Scotland’s Ear Reconstruction Service, Ken Stewart, left.Ken Stewart examining a patient, right.
For years, Ken had employed a number of techniques for approximating the varying circuitous designs of his patients’ ears. The most popular method is to borrow cartilage from the patients ribs and to carve this into an ear shape. Sometimes he practices or teaches using other materials such as wax, silicone, and even apples. “I love making ears,” he says in an interview with The Scotsman. In 2014, he began investigating 3D imaging solutions in an effort to streamline the pre-operative procedure for ear reconstructions. Ken admits, “With all the technology around us we need[ed] to improve this workflow. The ear reconstruction team at the Royal Hospital for Sick Children were keen to find new technologies to help.” Though Lothian NHS, where Ken is based, had already been using 3D imaging systems to design prosthetic limbs and carry out medical examinations, they wanted to improve the details of their reconstructed ears.
It was then that Ken decided to turn to Patrick Thorn & Co., Artec’s UK gold partner. Drawing from his extensive experience with designing and re-designing ear prosthetics and implants, Ken remained skeptical that Artec’s state-of-the-art scanners could effectively 3D render the human ear. To prove to Ken otherwise, Patrick decided to produce a range of sample replicas to demonstrate Artec’s high-resolution imaging capabilities. Patrick arranged to have the ears of his neighbors and grandson scanned. Following a few imaging modifications with the help of Leios Elaborations Scanning Software from EGS, he ordered the samples printed on the Roland ARM-10 3D Printer. Thrilled by the results, Ken and his team knew that they had to have an Artec Spider – a high-resolution 3D scanner that is well-suited for capturing images of deeper surfaces within the ear canal as well as around the area between the ear and the head.
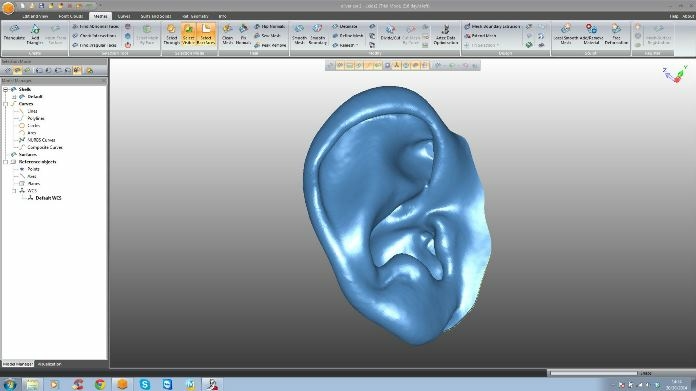

Modifications made using Leios.
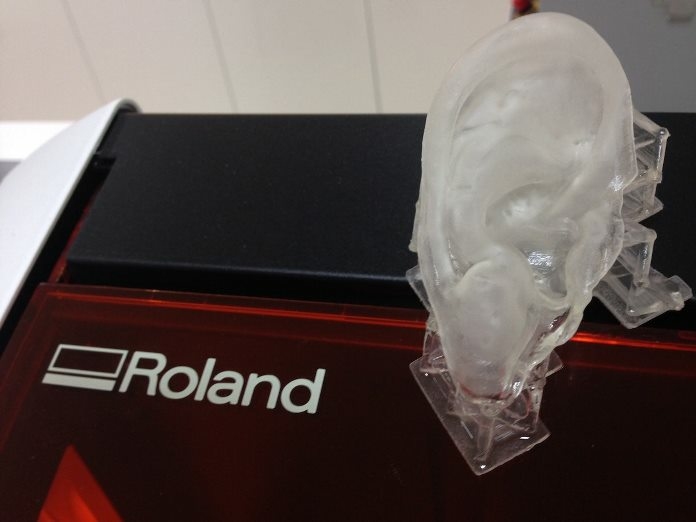
Pre-printing adjustments in Roland.
With the successful fundraising efforts of the Sick Kids Friends Foundation, The Royal Hospital for Sick Children purchased an Artec Spider, with Artec Studio and the Roland ARM-10. In a single afternoon, it was installed, and on the next day, hands-on training followed. Ken remarks, “Starting with exterior 3D scanning was new for us and as we have busy schedules with day-to-day patients, it has taken a little time to perfect. However, with the training and additional notes Patrick provided, we can now use the solution from scanning to 3D print with relative ease. The model is then sterilized and utilized in theater to improve the accuracy of our surgical reconstruction.”
Integrating Artec Spider into Ken’s ear reconstruction practice has both simplified and systemized the ear-building process. Once the initial consultation with patients concludes, they return to the hospital to have their unaffected ear scanned. In Ellie’s case, because she was diagnosed with bilateral microtia (meaning both ears are affected), the ear of her sister, who does not suffer from microtia, was scanned instead. Sometimes an image of the affected ear is also taken for reference. During the scanning, Artec Spider gets to work on capturing in striking detail the complex structure of the outer ear, and then probes deep into the ear canal, collecting further, invaluable visual data. Afterwards, the images are uploaded into Artec Studio, where they are swiftly aligned, and fused to construct an impressive 3D digital model of the ear.
During the retouching stage, Leios is used to check the ear’s surface, remove any unnecessary elements, and allow for skin thickness by applying an internal offset. Once all the structural and cosmetic alterations have been finalized, the resulting image is mirrored. Thereafter, an electronic file containing the images is delivered via a shared drive to a laboratory and loaded onto the Roland MonoFab Printing Software, in which alignments are performed. All that’s left is to press “Go” to start 3D printing.

Jeff Millar, Consultant Maxillofacial Prosthetist, preparing to 3D print the ears on the Roland MonoFab.
The printed result.
After about three hours, the reproduced ears are readied out of the 3D printer by being washed in isopropanol. And for a few minutes, they are left to sit under a UV lamp to harden into their shape. They are then sterilized, sealed, and sent to the operating room to serve as 3D templates for ear reconstruction.
It might be said that ear reconstruction has developed slowly (albeit steadily) over the last forty years that plastic surgeons have been trying to perfect it. It began in the 1970s with surgeons extracting cartilage from the rib to be used as the tissue base for reconstructing the ear. At the time, a 2D paper tracing of the normal ear helped guide the surgeon shape the extracted cartilage into some semblance of the patient’s future ear. But, such a graphic model served merely as an approximation. The complex dimensions of the ear, however, require nothing short of precision. With the help of advanced imaging solutions from Artec3D, surgeons like Ken can rest assured that they’ll never have to approximate models for the prosthetics and implants they create, especially when their patients are kids like Ellie.
Moving forward the team is collaborating with the Centre for Regenerative Medicine at Edinburgh University, where Professor Bruno Peault and Dr Chris West have successfully isolated human stem cells from fat. These purified stem cells have been tried against a library of 10,000 FDA approved polymers. Dr West identified several to which the stem cells will bind. The cells can then be driven to produce cartilage on the polymer surface. The hope is that by combining Artec 3D scanning technology with tissue engineering technology and a bit of liposuction it will be possible to produce truly bespoke mirror image replicas of the opposite ear which can be implanted and thus avoid the need for using rib cartilage.


The 3D print that served as a reference to design Ellie's ear implant.
The ear up close.
As the technology and skills are ever increasing in the NHS Lothian, the staff and patients at the Royal Hospital for Sick Children are looking forward to moving into their new purpose-built home at Little France, Edinburgh, in autumn 2017, where more 3D related work will continue.
Special thanks to Ellie and her mum for allowing us to share this success story.



